Race and ethnicity are determining flu vaccine rates in Medicare
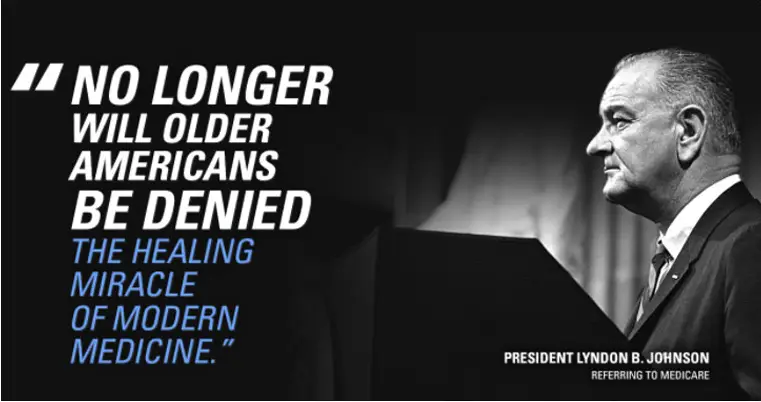
Medicare Program
On July 30, 1965, President Lyndon B. Johnson signed into law the Social Security Act Amendments, popularly known as the Medicare bill. It established Medicare, a health insurance program for the elderly.
In the 1990s Medicare managers decided that fulfilling the mandate of providing health care security to Medicare beneficiaries required assurances that taxpayer dollars were used effectively and that beneficiaries received care consistent with medical quality standards.
STRUCTURAL RACIAL INEQUALITY
A recent article and commentary in the British Journal Lancet Healthy Longevity found racism “as the originating factor” determining differences in vaccine rates between whites and minorities in Medicare, rather than social class. “Structural racial inequity”, the commentator concluded, “…should be included in any discussion of structural interventions”. The authors of the article for their part concluded “New legislative, fiscal, and educational strategies are urgently needed to address these inequities.”
Medicare Fails
Evidence from the Lancet report shows that Medicare program managers have historically failed to ensure quality medical standards are applied to the care given to minority Medicare beneficiaries.
They have permitted the race of the beneficiaries to inform the care that is being delivered.
Trends in the administration of the influenza vaccine is an example of racism in the program. It is time to change the inequities within health care.

“There is nothing more unequal than the equal treatment of unequal people.”
Unequal Treatment
African American and Hispanic Medicare beneficiaries are at heightened risk for severe influenza because they are significantly less likely than white people to receive seasonal influenza vaccines.
This unequal treatment has been documented and has been occurring for over 20 years.
Even when vaccinated minority Medicare beneficiaries, including Asian Americans, are routinely administered a less effective flu vaccine.
Historic Inequities
These differences cannot be explained away by vaccine hesitancy among minorities, or by variations in the social determinants of health and health literacy between whites and people of color.
The cause for the difference in vaccine rates is racism in the Medicare program.
The program’s failure to address the underlying cause of this inequity has contributed to:
Non-Hispanic Black people had the highest flu-related hospitalization rate (69 per 100,000)
Non-Hispanic American Indian or Alaska Native people had the second-highest flu-related hospitalization rate (49 per 100,000)
Hispanic or Latino people had the third-highest flu-related hospitalization rate (45 per 100,000)
Non-Hispanic White people had a lower flu-related hospitalization rate (38 per 100,000) compared with these three groups

Paradigm Shift
Medicare needs to be reimagined so that mitigation of beneficiary risk is the prime directive of the program.
No Medicare policy cannot elevate a beneficiary risk for a poor health outcome.
Medicare needs to ensure that there are no inequities in the quality of care delivered to Medicare beneficiaries by age, gender, sexual orientation, or race and ethnicity.
Where inequities are found, Medicare needs to develop and execute a plan to eliminate them with all deliberate speed.
CLICK HERE TO LEARN MORE ABOUT OUR CAPABILITIES