
Maternal Health: Terminology
Cardiomyopathy – A disease of the heart muscle that makes it harder for the heart to pump blood to the rest of the body. Cardiomyopathy can lead to heart failure.
Doula – A professional birthing coach. Can assist with childbirth, postpartum, or the full spectrum of maternal health.
Hemorrhage – Bleeding from a damaged blood vessel.
High-risk Pregnancy – When the birthing person or baby are at an increased risk of a health problem.
Hypertension – High blood pressure.
Low Birth Weight – A term used to describe an infant born weighing 5.5 pounds (2500 grams) or less.
Maternal Mortality – The death of a woman during pregnancy, at delivery, or soon after delivery is a tragedy for her family and for society as a whole.
Maternal Health – Refers to the health of women during pregnancy, childbirth, and the postnatal period.
Preterm Birth – Refers to birth before 37 weeks of gestation. Also called “premature”.
Preterm Labor – Labor that begins before the 37th week of pregnancy.
Pulmonary Embolism – A blockage in one of the pulmonary arteries in your lungs.
Sources: Hemorrhage: What is it, causes & when to call the doctor. Cleveland Clinic. (n.d.). Retrieved May 5, 2022, from https://my.clevelandclinic.org/health/symptoms/21654-hemorrhage Mayo Foundation for Medical Education and Research. (2020, June 13). Pulmonary embolism. Mayo Clinic. Retrieved May 5, 2022, from https://www.mayoclinic.org/diseases-conditions/pulmonary-embolism/symptoms-causes/syc-20354647 Mayo Foundation for Medical Education and Research. (2022, April 2). Cardiomyopathy. Mayo Clinic. Retrieved May 5, 2022, from https://www.mayoclinic.org/diseases-conditions/cardiomyopathy/symptoms-causes/syc-20370709 Metzger, G. K. (n.d.). Pregnancy glossary. WebMD. Retrieved May 5, 2022, from https://www.webmd.com/baby/pregnancy-glossary NCI Dictionary of Cancer terms. National Cancer Institute. (n.d.). Retrieved May 5, 2022, from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/low-birth-weight World Health Organization. (n.d.). Maternal health. World Health Organization. Retrieved May 5, 2022, from https://www.who.int/health-topics/maternal-health#tab=tab_1
Maternal Health Inequities
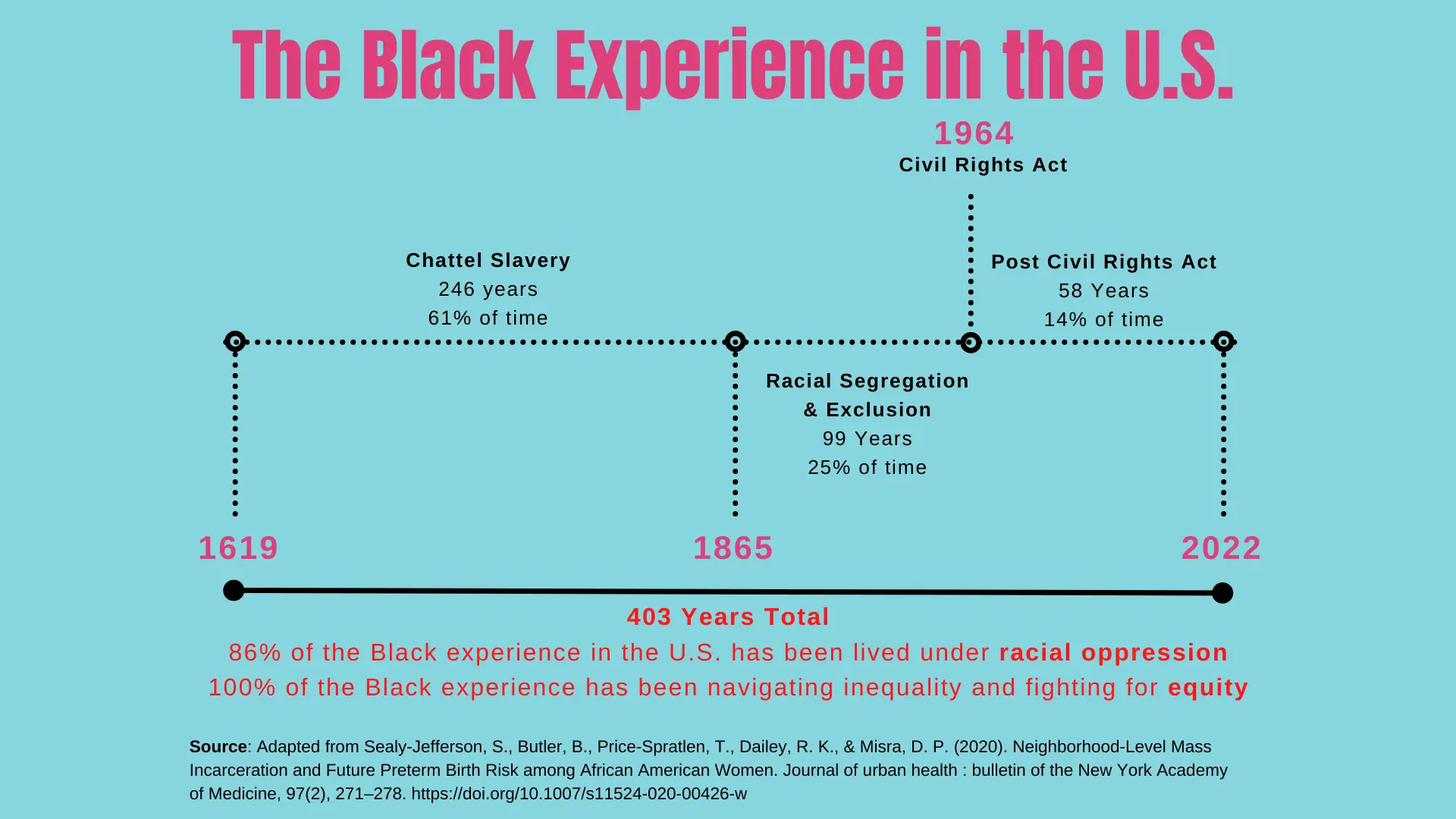
Maternal Health Inequities: Historical Context
- Black women were used to perpetuate the institution of slavery by being forced into birthing more enslaved peoples (1)
- Modern gynecology was built on the backs of enslaved women like Anarcha, Betsey, and Lucy under forced experimentation by Dr. J Marion Sims (2)
- Black women were often forced to breast feed and care for white babies while having their own children stripped from them and sold to other enslavers (3)
1. Roberts, D. E. (1999). Killing the black body: Race, reproduction, and the meaning of Liberty. Vintage. 2. Wall LL. J Med Ethics. 2006;32(6):346-350. 3. Muse, S. (2021, February 1). Breastfeeding America: What we know. MomsRising. Retrieved April 19, 2022, from https://www.momsrising.org/blog/breastfeeding-america-what-we-know
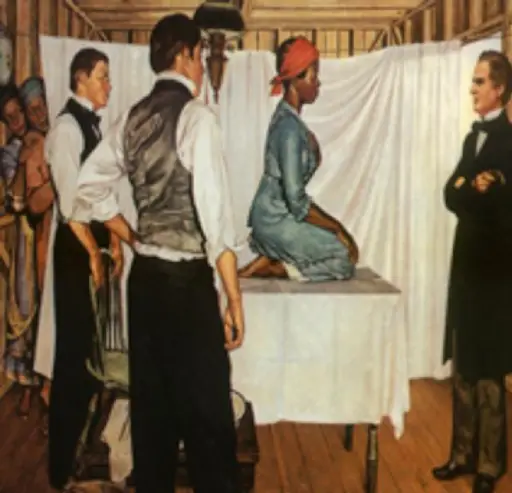
Illustration of Dr. J. Marion Sims with Anarcha by Robert Thom. Anarcha was subjected to 30 experimental surgeries. Pearson Museum, Southern Illinois University School of Medicine
Maternal Health Inequities: The Problem
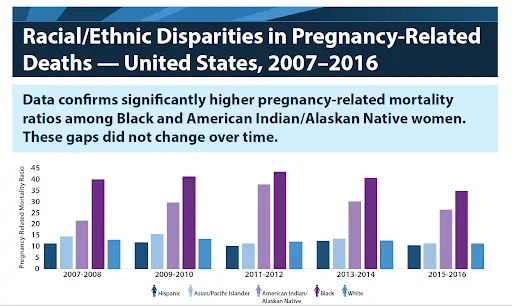
Maternal Mortality Rates
- About 700 women die in the U.S. each year as the result of pregnancy or pregnancy-related complications
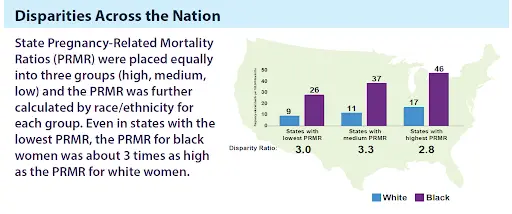
- Black women have pregnancy-related mortality rates that are 3x higher than that of white women (see Figure 1 from Kaiser Family Foundation)
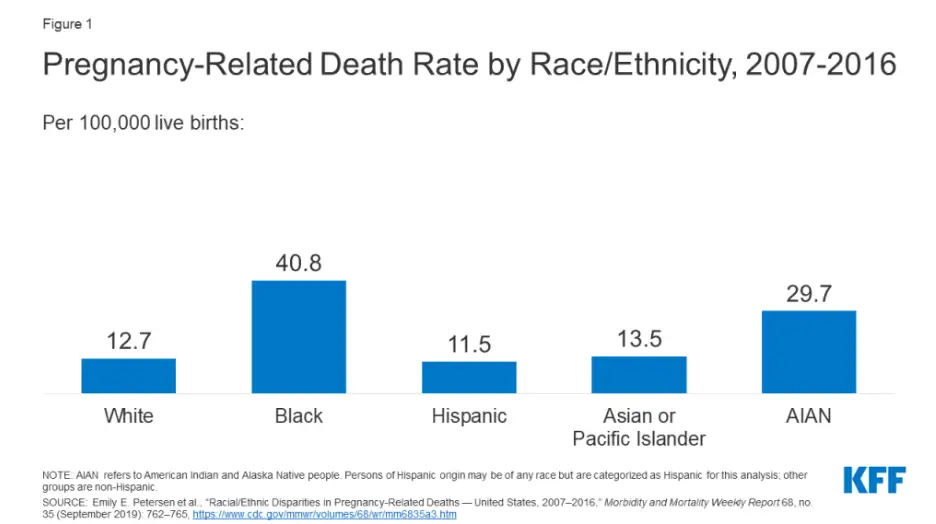
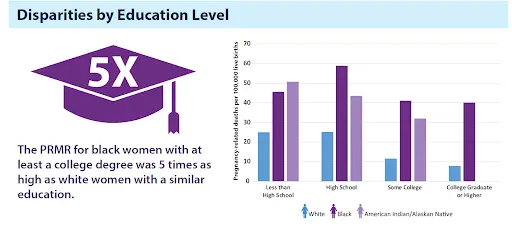
- These inequities persist across education levels and socioeconomic status
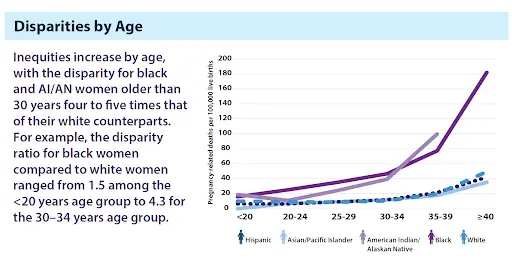
- Inequities in maternal mortality increase with maternal age
- Per KFF: “Notably, the pregnancy-related mortality rate for Black women with a completed college education or higher is 1.6 times higher than the rate for White women with less than a high school diploma.”
- Most pregnancy-related mortality is preventable, and therefore unnecessary, underscoring the persistence of inequities
1.Artiga, S., Pham, O., Orega, K., & Ranji, U. (2020). Racial Disparities in Maternal and Infant Health: An Overview - Issue Brief. Retrieved 9 May 2022, from https://www.kff.org/report-section/racial-disparities-in-maternal-and-infant-health-an-overview-issue-brief/
Maternal Health Inequities: Birth Risk and Outcomes
- Cardiomyopathy
- Pulmonary Embolism
- Hypertension (High Blood Pressure)
- Hemorrhage

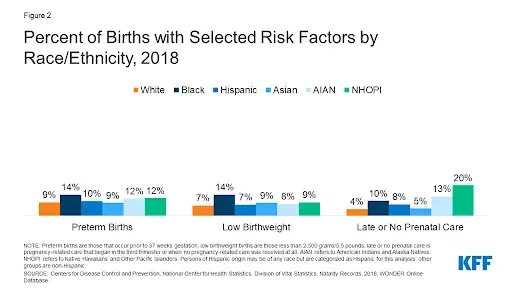
- Black women are more likely to have birth risk factors
- Preterm birth
- Low birthweight
- Births for which they received late or no prenatal careHispanic women also are twice as likely compared to White women to have a birth with late or no prenatal care compared to White women (8% vs. 4%)
Hispanic women also are twice as likely compared to White women to have a birth with late or no prenatal care compared to White women (8% vs. 4%)
Maternal Health Inequities: Infertility Rates
The CDC reports that among heterosexual women in the U.S. aged 15 to 49 years with no prior births, approximately 19% are unable to become pregnant after one year of trying. Within this group of women, approximately 26% not only have difficulty getting pregnant, but also have a hard time carrying a pregnancy to full term.
The CDC also reports that among women with one or more prior births, 6% aged 15 to 49 years and who are married are unable to get pregnant. Conversely, 14% of this group have a difficult time carrying a person to term.
Centers for Disease Control and Prevention. (2022, March 1). Infertility. Centers for Disease Control and Prevention. Retrieved May 5, 2022, from https://www.cdc.gov/reproductivehealth/infertility/index.htm#:~:text=In%20the%20United%20States%2C%20among,to%20term%20(impaired%20fecundity).

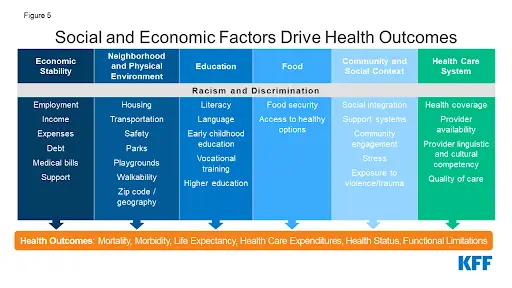
Maternal Health Inequities: Drivers of Inequities
- Drivers of Inequities
- Institutional Racism
- Class Oppression
- Gender Exclusion, Discrimination, and Exploitation
- Social, Political, and Systemic Determinants of Health
- Increased health risk factors
- Late or no prenatal care
- Quality labor and delivery care
- Patient education
- Provider education
- Implicit Bias
- All contribute to the decline in health outcomes and psychosocial stress of the Black community, creating inequitable health outcomes

- Challenges for Birthing People to Stay Safe from Vaccine-Preventable Diseases:
- Isolation for avoiding infections
- Access to quality health care
- Access to certain vaccinations
- Vaccine hesitancy
- Inaccurate information on social media
- Expectations regardless of individual health conditions, concerns, and societal stigmas
- Shortage of vaccines on-hand at clinics, leading to pharmacy referrals
- Risk of severe disease if unvaccinated
- Provider withholding vaccine recommendations, especially for birthing people of color
- Misconceptions on safety of vaccines
Maternal Health Inequities: Resources
Articles
Maternal Health & Vaccines
- The Centers for Disease Control and Prevention (CDC) recommend all people planning to be pregnant receive their MMR vaccination before becoming pregnant to protect against rubella.
- Out of an abundance of caution, it is best to avoid becoming pregnant, if possible, until one month after receiving the MMR vaccine and your immunity is confirmed by a blood test.
- A pregnant person should get vaccinated against whooping cough (also known as Tdap) and flu during each pregnancy to protect herself and her baby, with immunity for the first few months of life.
- Pregnant people are more likely to get severely ill with COVID-19 compared with non-pregnant people. If you are pregnant, you can receive a COVID-19 vaccine. Getting a COVID-19 vaccine during pregnancy can protect you from severe illness from COVID-19. If you have questions about getting vaccinated, talk to your healthcare provider.

- Some pregnant people may be recommended for meningococcal vaccination by their doctor if they work in a lab or are traveling to a place where they may be exposed to the disease.
- Some pregnant people may need the hepatitis B vaccination or the hepatitis A vaccination as recommended by their doctor.
- Take the Following Risk Mitigation Measures:
- Vaccination
- Ventilation
- Wear a mask
- Practice good hand hygiene
- Practice social and physical distancing
- Avoid crowded situations regardless of community transmission levels
- Don’t allow touching of you or your baby
Maternal Health & Vaccines: The Flu Vaccine
- Pregnant people are more likely to have severe illness from flu, possibly due to changes in immune, heart, and lung functions during pregnancy.
- A prospective cohort study from November 2020 – March 2021 showed that Black, Indigenous, and other People of Color (BIPOC) who were pregnant were 80% less likely to have flu vaccine acceptance and more than 70% less likely to COVID-19 vaccinations^1
- Make sure to receive your yearly flu vaccine —it’s the best way for a pregnant woman to protect against the flu and protect the baby for several months after birth from flu-related complications.
- CDC recommends getting a flu vaccine by the end of October despite flu seasons varying in their timing from season to season. This timing helps protect a pregnant woman before flu activity begins to increase.
1. Unger, R., Hamm, R. F., Triebwasser, J. E., Trout, K. K., Levine, L. D., & Dolin, C. D. (2022). Racial disparities in acceptability of maternal influenza and covid-19 vaccination. American Journal of Obstetrics and Gynecology, 226(1). https://doi.org/10.1016/j.ajog.2021.11.508 2. https://www.cdc.gov/flu/highrisk/pregnant.htm


- Flu vaccination coverage for pregnant persons 18 to 49 years:
- 9.1 percentage points lower this season as of February 2022 compared with last season at the end of February 2021 (51.7% compared to 60.8%)
- Coverage this season as of February 2022 is 22.2% percentage points lower for non-Hispanic Black pregnant persons than non-Hispanic White pregnant persons (30.2% compared to 52.4%)
- Flu vaccination coverage for pregnant persons 18 to 49 years is lower for all race/ethnicity groups as of the end of February 2022 compared with the end of February 2021:
- 6.0 percentage points lower for non-Hispanic Black pregnant persons (30.2% compared to 36.2%)
- 8.6 percentage points lower for non-Hispanic White pregnant persons (52.4% compared to 61.0%)
- 11.2 percentage points lower for Hispanic/Latino pregnant persons (50.8% compared to 62.0%)
- 9.3 percentage points lower for non-Hispanic Other race/ethnicity pregnant persons (50.3% compared to 59.6%)
- 8.4 percentage points lower for non-Hispanic Asian pregnant persons (68.0% compared to 76.4%)
Weekly Flu Dashbaord. (2022). Retrieved 9 May 2022, from https://www.cdc.gov/flu/fluvaxview/dashboard/vaccination-dashboard.html
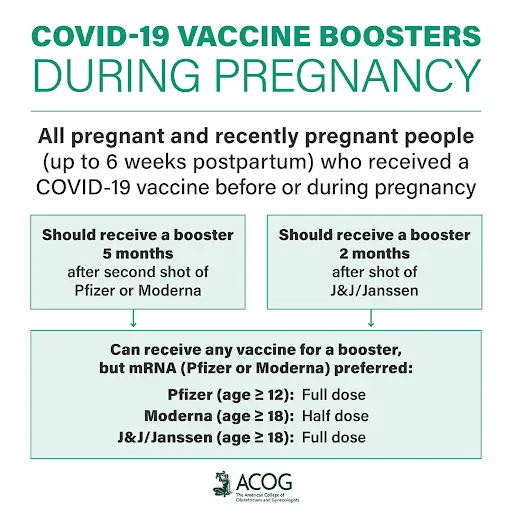
Maternal Health & Vaccines:
The COVID-19 Vaccine & Boosters
Pregnant people are more likely to get severely ill with COVID-19 compared with non-pregnant people. If you are pregnant, you can receive a COVID-19 vaccine. Getting a COVID-19 vaccine during pregnancy can protect you from severe illness from COVID-19. If you have questions about getting vaccinated, talk to your healthcare provider.
Also, a COVID-19 vaccination of the mother may protect the newborn against COVID-19 hospitalization.
Halasa NB, Olson SM, Staat MA, et al. Effectiveness of Maternal Vaccination with mRNA COVID-19 Vaccine During Pregnancy Against COVID-19–Associated Hospitalization in Infants Aged <6 Months — 17 States, July 2021–January 2022. MMWR Morb Mortal Wkly Rep 2022;71:264–270. DOI: http://dx.doi.org/10.15585/mmwr.mm7107e3
Maternal Health & Vaccines:
COVID-19 in Pregnancy
COVID-19 during pregnancy is associated with severe illness and death, and pregnant women with COVID-19 are more likely to experience preterm birth, stillbirth, and other pregnancy complications.
Vaccination is recommended for pregnant women to prevent COVID-19, including severe illness and death. COVID-19 vaccination is safe and effective when administered during pregnancy. Receipt of COVID-19 vaccination during pregnancy is associated with detectable maternal antibodies in maternal sera at delivery, breast milk, and infant sera indicating transfer of maternal antibodies.

One study, in the Netherlands, showed pregnant women infected with COVID-19, had an increased hospital/ICU admission and need for cesarean section. In the same study, Minorities and those who are overweight/obese had a higher risk factor of severe COVID-19 complications including infection in pregnancy, risk of cesarean section and hospital and intensive care unit.
1. Morgan, J. A., Biggio, J. R., Jr, Martin, J. K., Mussarat, N., Chawla, H. K., Puri, P., & Williams, F. B. (2022). Maternal Outcomes After Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Vaccinated Compared With Unvaccinated Pregnant Patients. Obstetrics and gynecology, 139(1), 107–109.
2. Morgan, John A. MD; Biggio, Joseph R. Jr MD, MS; Martin, Jane K. MD; Mussarat, Naiha MD; Chawla, Harsheen K. BSc; Puri, Priya BSc; Williams, Frank B. MD Maternal Outcomes After Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Vaccinated Compared With Unvaccinated Pregnant Patients, Obstetrics & Gynecology: January 2022 - Volume 139 - Issue 1 - p 107-109
doi: 10.1097/AOG.0000000000004621
3. Overtoom, E. M., Rosman, A. N., Zwart, J. J., Vogelvang, T. E., Schaap, T. P., van den Akker, T., & Bloemenkamp, K. (2022). SARS-CoV-2 infection in pregnancy during the first wave of COVID-19 in the Netherlands: a prospective nationwide population-based cohort study (NethOSS). BJOG : an international journal of obstetrics and gynaecology, 129(1), 91–100. https://doi.org/10.1111/1471-0528.16903
Copy
Download .nbib
Format:
4. Shook LL, Atyeo CG, Yonker LM, et al. Durability of Anti-Spike Antibodies in Infants After Maternal COVID-19 Vaccination or Natural Infection. JAMA. 2022;327(11):1087–1089. doi:10.1001/jama.2022.1206
5. Halasa NB, Olson SM, Staat MA, et al. Effectiveness of Maternal Vaccination with mRNA COVID-19 Vaccine During Pregnancy Against COVID-19–Associated Hospitalization in Infants Aged <6 Months — 17 States, July 2021–January 2022. MMWR Morb Mortal Wkly Rep 2022;71:264–270. DOI: http://dx.doi.org/10.15585/mmwr.mm7107e3external icon
Maternal Health & Vaccines:
Common Myths – COVID-19 Vaccines
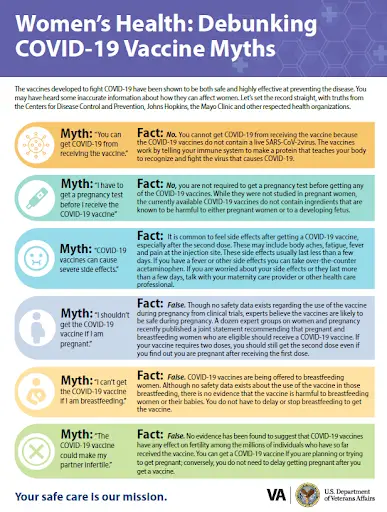
Multiple studies have shown that people who have received flu shots during pregnancy have not had a higher risk for spontaneous abortion (miscarriage). One of the largest and strongest studiesexternal icon was conducted in CDC’s Vaccine Safety Datalink (VSD) project. The recently published study covered three flu seasons (2012-13, 2013-14, 2014-15) looking for any increased risk for miscarriage among pregnant people who had received a flu vaccine during their pregnancy. The study found NO increased risk for miscarriage after flu vaccination during pregnancy.
This study was conducted in follow-up to a previous smaller study. The prior studyexternal icon examined data from the 2010-2011 and 2011-2012 flu seasons and identified an association between flu vaccination early in pregnancy and an increased risk of spontaneous abortion or miscarriage; particularly among people who had received flu vaccine during the previous flu season. However, the smaller study had several limitations, including small sample size which could have led to imprecise results. This study was the only analysis to show that association; no other studies had found an increased risk of SAB following flu vaccination At this time, the Advisory Committee on Immunization Practices (ACIP), the American College of Obstetricians and Gynecologists (ACOG)external icon and CDC continue to recommend that pregnant people get a flu vaccine during any trimester of their pregnancy because flu poses a danger to pregnant people and a flu vaccine can prevent serious illness, including hospitalization, during pregnancy.
Maternal Health & Vaccines: Additional Resources
Maternal Health: Perspectives from Birthing People and Doula's
Meet Samantha Griffin, CEO and Owner of DC Metro Maternity and Doula.
In this video, Samantha outlines the importance of maternal care in the Black community from the valuable perspective of a doula.
Samantha was also a panelist during the Health Champions webinar, “Maternal Health and Vaccines.”
Meet Falasha Zuend, soon-to-be mother of three and birthing person.
In this video, Falasha outlines the importance of health and vaccines during pregnancy from the perspective of an African American woman.
Falasha was also one of the panelists during the Health Champions webinar, “Maternal Health and Vaccines”
Maternal Health: Presence of a Doula
Systemic racism’s prevalence in healthcare underscores the need for Black and Hispanic/Latinx birthing people to have a strong advocate during their birthing experience.
- Doulas, midwives, and birth support workers are uniquely positioned to fill this role
- Types of Doulas According to the National Black Doulas Association®
- Childbirth: a person experienced in childbirth who provides advice, information, emotional support, and physical comfort to a mother before, during, and immediately after childbirth.

- Postpartum: a person who provides evidenced based information on things such as infant feeding, emotional and physical recovery from birth, mother–baby bonding, infant soothing, and basic newborn care. A postpartum doula is there to help a new family in those first days and weeks after bringing home a new baby.
- Full Spectrum: a growing group of Doulas and justice rights advocates who are working to bring the Doula care model to people across the full spectrum of pregnancy issues, including abortion, stillbirth and miscarriage, fertility and sex.
1.Salinas, J. L., Salinas, M., & Kahn, M. (2022). Doulas, Racism, and Whiteness: How Birth Support Workers Process Advocacy towards Women of Color. Societies, 12(1), 19. MDPI AG. Retrieved from http://dx.doi.org/10.3390/soc12010019
https://www.mdpi.com/2075-4698/12/1/19/htm,
2. National Black Doulas Association®. (2022). Retrieved May 2022, from https://www.blackdoulas.org/
Certification
- The National Black Doulas Association® offers training and certification as a doula.
- Certification Dashboard
NOTE: In 2021, HealthLaw.org found that the following states reimbursed for doula services through Medicaid: Florida, Minnesota, New Jersey, and Oregon.
Robles-Fradet, A. (2022, April 1). Medicaid coverage for Doula Care: State Implementation Efforts. National Health Law Program. Retrieved May 5, 2022, from https://healthlaw.org/medicaid-coverage-for-doula-care-state-implementation-efforts/#:~:text=Our%20current%20efforts%20to%20track,%2C%20New%20Jersey%2C%20and%20Oregon.
Resources for Birthing People & Doulas
Policy Implications for Maternal Health Inequities
- Madame Vice President Kamala Harris has issued a call to action on maternal health
- 11 Additional States and D.C. Ask to Extend Medicaid and CHIP Coverage to a Full Year After Pregnancy under American Rescue Plan
- CMS is proposing the “Birthing-Friendly” hospital designation to drive improvements in maternal health outcomes and maternal health equity
- CMS will convene health care industry stakeholders – including health care facilities, insurance companies, state officials and providers – to focus on industry commitments to improve health outcomes experienced by pregnant and postpartum people
- The Department of Health and Human Services (HHS), through the Health Resources and Services Administration (HRSA), announced approximately $16 million to strengthen Maternal, Infant, and Early Childhood Home Visiting (MIECHV) Programs through seven awards supporting eight states
- State Maternal Health Innovation and Implementation (State MHI) Program
- HS, through the Health Resources and Services Administration (HRSA), is also, on telehealth.hhs.gov, posting a new Maternal Health Best Practice Guide for providers to incorporate telehealth for prenatal and postpartum care, and monitoring within high-risk pregnancy.
- HHS announced $4.5 million in funding for investing in doulas
Policy Implications for Maternal Health Inequities: Resources
Watch Now: Black Maternal Health & Vaccines
NMQF’s Center for Sustainable Health Care Quality and Equity (SHC) hosts a Health Champions discussion on “Champions for Total Health: Black Maternal Health & Vaccines” with a focus on flu and COVID-19 vaccination rates among pregnant people of color.
Panelists:
Carla S. Rogers-Henry, MD, MA, Assistant Professor of Obstetrics & Gynecology, Icahn School of Medicine at Mount Sinai, Chief of Ambulatory Women’s Health Services Obstetrics & Gynecology, Elmhurst Hospital Center
Lois Privor-Dumm, IMBA Director, Adult Vaccines International Vaccine Access Center ,Johns Hopkins University Bloomberg School of Public Health
Samantha Griffin Owner, Doula DC Metro Maternity
Falasha Zuend, Birthing Person
Brittani Nelson, MPH Program and Policy Coordinator Louisiana Cancer Prevention & Control Programs (LCP) LSU Health New Orleans (Moderator)
Share Your Birthing Story or Experience
