Hypertension Defined
What is Hypertension?
- Also known as high blood pressure or the “silent killer”, hypertension is a condition where the blood moving from the heart to the body is pumped under high pressure. This can damage the organs and cause wear on the heart
- Blood pressure = amount of blood pumped by the heart + amount of resistance (push back) to blood flow in the arteries
- More blood pumped by the heart coupled with more narrow arteries leads to higher blood pressure
- It’s measured in millimeters of mercury (mm Hg) and written as two numbers (for example, 112/78 mm Hg)
- The top number – systolic pressure – is the pressure when the heart beats
- The bottom number – diastolic pressure- is the pressure when the heart rests between beats
(High blood pressure (hypertension) 2021)
Healthy & Unhealthy Blood Pressure Ranges
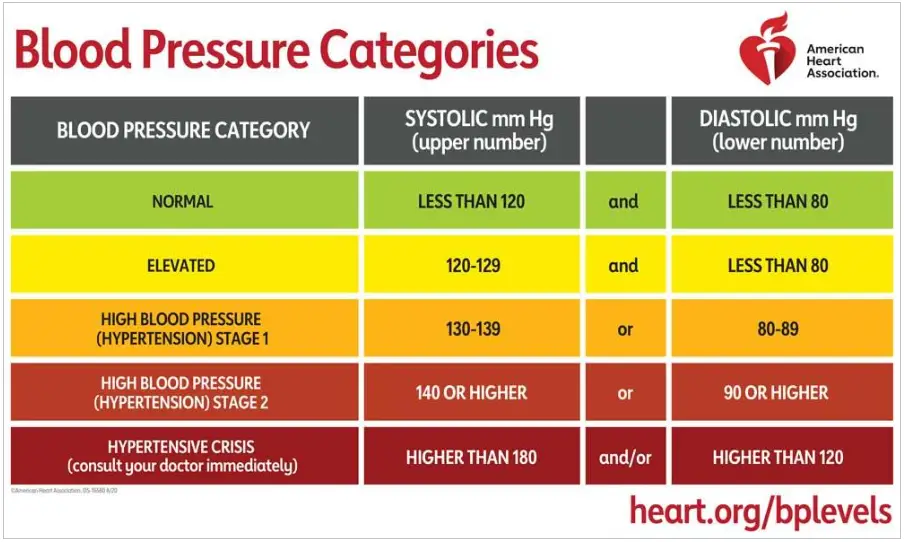
(Understanding blood pressure readings 2022)
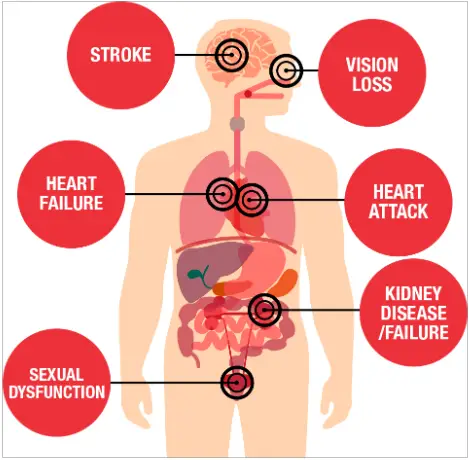
The Silent Killer
- Consistent high blood pressure can be harmful
- Many people do not know they have high blood pressure
- High blood pressure makes the heart work too hard and damages the blood vessels
- The results, over time, include heart failure, heart attack, kidney disease, stroke, and vision loss
- Knowing your numbers and making changes that can prevent or treat high blood pressure are keyany

(What is high blood pressure? 2021)
American Heart Association Graphic of Potential Health Issues due to Hypertension
(What is high blood pressure? 2021)
Lifestyle Drivers of Hypertension
Screening
(Cdc, 2022)
Inequities in Hypertension Outcomes
Inequities in Hypertension Outcomes
- Disparate outcomes in hypertension are prevalent among historically excluded communities
- Researchers studying the racial and ethnic differences in hypertension prevalence, awareness, treatment, and control found that Black adults living in the US between 2013 – 2018 have a higher hypertension prevalence than white adults (45.3% versus 31.4% respectively) but have similar awareness and treatment rates as white adults.
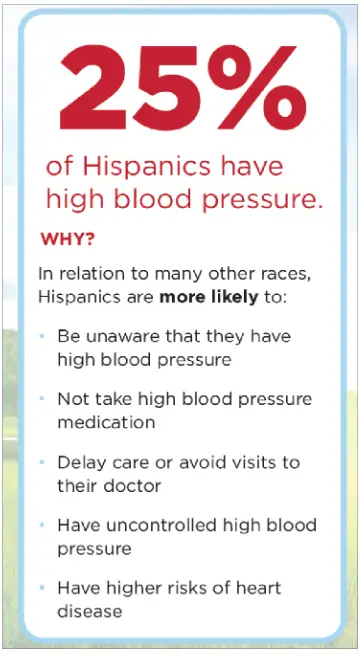
- Conversely, Hispanic adults have similar hypertension prevalence and treatment rates than white non-hispanic adults, but lower awareness (71.1% awareness in Hispanic adults versus 79.1% awareness in white adults)

(Aggarwal et al., 2021)
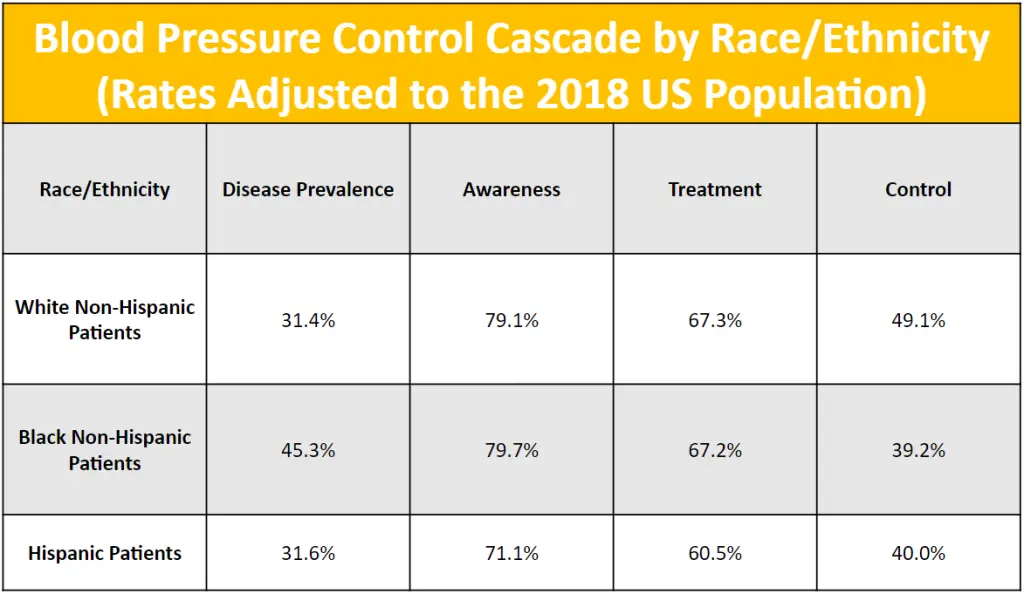
(Aggarwal et al., 2021)
Black Americans and Hypertension
- Black Americans in the U.S. have a higher prevalence of high blood pressure (HBP) than other racial and ethnic groups
- It is also often more severe in Black patients and some medications are less effective in treating Black patients with HBP
- Unfortunately, death due to hypertensive heart disease is nearly two times higher among Black patients than white patients
- Likewise, poorly controlled blood pressure during pregnancy and after childbirth is a leading reason Black women experience higher rates of pregnancy-related death than white women
(Minority health month: Spotlight on hypertension 2022)

(National Hypertension Control Initiative: Printable Resources)
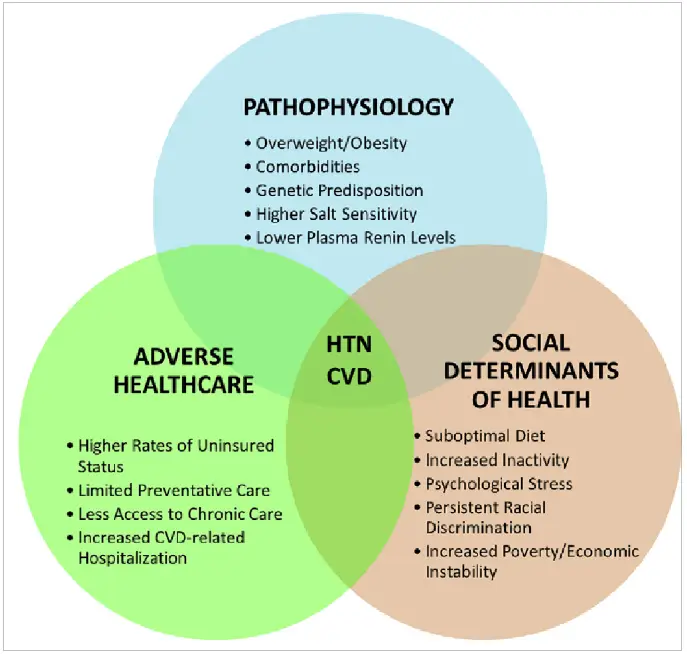
Drivers of Inequities in Hypertension
- Researchers have also worked to identify the drivers of inequities in hypertension outcomes
- The 4th Annual University of Utah Translational Hypertension Symposium discussed the intersections of the COVID-19 pandemic, hypertension and preexisting disparities in hypertension that were exacerbated by the pandemic
(Bress et al., 2021)
- Factors that emerged from this discussion include:
- Structural racism
- The digital divide (e.g., unequal access to hi-speed internet and unequal digital literacy)
- Lack of access to health insurance and/or healthcare
- Lack of access to a built environment that empowers physical activity
- Food insecurity
- Diets lacking nutrient-dense foods
- Resistant hypertension
- Low health literacy
- Distrust of the healthcare system
- Provider biases (clinical and cultural uncertainty, beliefs, and stereotypes about minority patients)
- Clinical inertia (clinicians’ failure to initiate or intensify antihypertensive therapy when BP goals are unmet)
- Resistant hypertension
- Earlier hypertension
(Ferdinand et al., 2020)
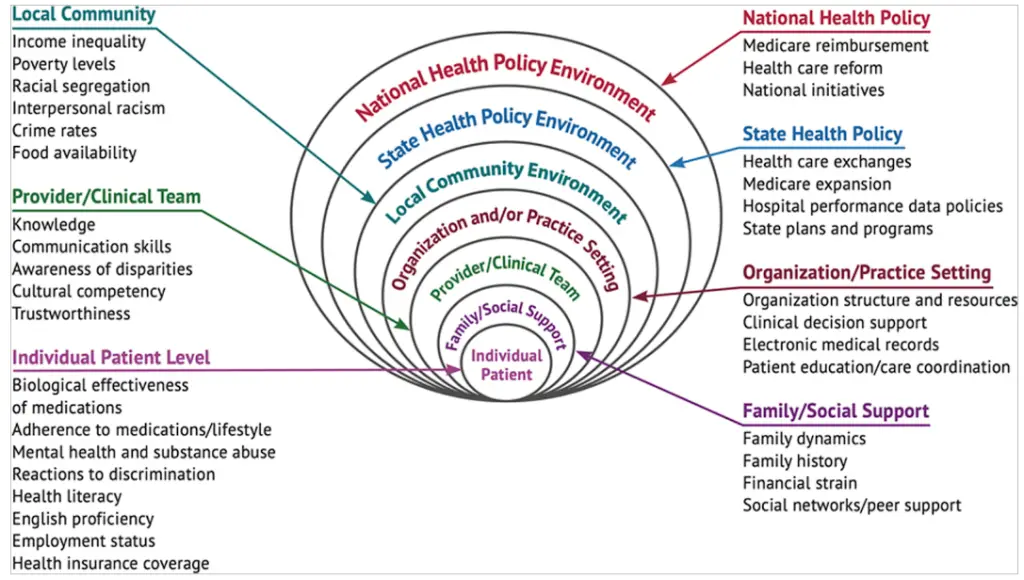
(Bress et al., 2021) Authors adapted with permission from Mueller et al., ©2015, Oxford University Press.
Hypertension and COVID-19
- According to a review recently published in 2021, hypertension was identified as the most prevalent cardiovascular comorbidity in patients infected with the SARS-CoV-2 virus that causes COVID-19
- Studies showed that a COVID-19 would “demonstrably” increase the risk of hospitalization and death due to hypertension

(Peng et al., 2021)
- Medications for high blood pressure do not increase the severity of COVID-19
- Being fully vaccinated and receiving all recommended boosters is the best protection against the risk of hospitalization and death from COVID-19 in patients living with hypertension
- Consult your physician with any questions or concerns you may have
- One study suggests that treating high blood pressure during the pandemic should involve telemedicine to manage the chronic illness
- It notes that effective management and treatment of high blood pressure will be key in fighting COVID-19
- Since racial and ethnic minorities are more likely to be hospitalized and/or die from COVID-19, and they often experience high blood pressure at higher rates, using new approaches like telemedicine will assist in fighting this illness
(Swamy et al., 2022)
Hypertension and Flu

- According to the AHA, patients living with high blood pressure have an increased risk of serious health issues due to flu
- Patients with heart disease are more likely to die from an infection with influenza than patients with any other chronic condition
- The AHA notes that flu symptom management is important, but understanding the risks of blood pressure elevation due to cold and flu medications is equally vital
- “The American Heart Association and the American College of Cardiology recommend that people with cardiovascular disease, including those with coronary and other atherosclerotic vascular disease, get a flu shot annually.”
- People age 65 and older should try to get the high dose flu shot
- Consult your physician with any questions or concerns you may have

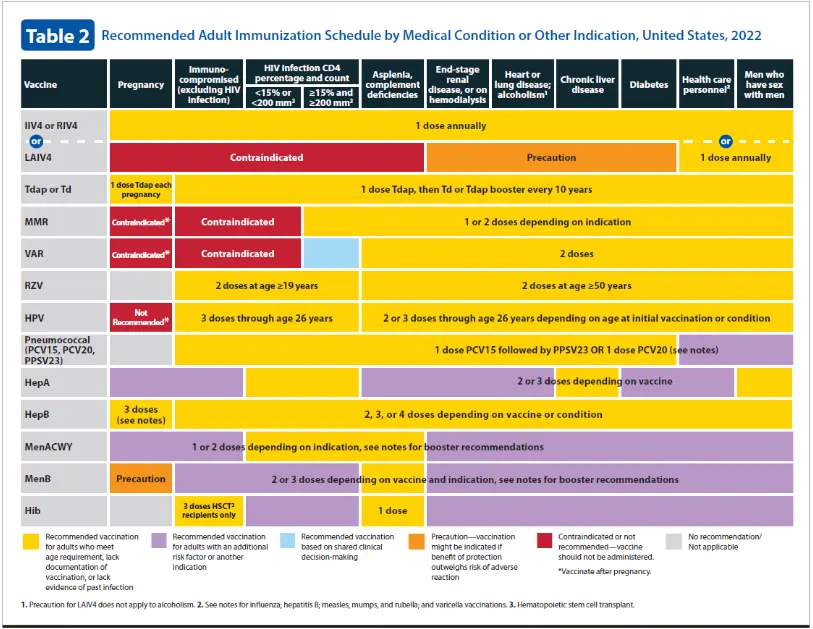
Hypertension and Adult Vaccines
Disparities may occur across the cancer continuum of care.
Additional Resources
Watch Now: Hypertension And Vaccines
Panelists:
Yabo Beysolow, MD, MPH, FAAP, COVID & Flu Immunization Expert, AIM and iREACH Program for Centers for Disease Control and Prevention
Dr. Yabo Beysolow is a pediatrician with over 20 years of experience in private practice and urgent care settings. She is also a public health professional with several years of work experience at the Centers for Disease Control and Prevention, CDC, in the Immunization Services Division, where Dr. Beysolow led as a Medical Officer and subject matter expert on immunizations, assisted in the development of and presented educational content for live, print, web-based, and remote audiences at the local, state and national levels. Dr. Beysolow led the U.S. Childhood Immunization Schedule Working Group from 2011-2014 as the CDC representative to the ACIP (Advisory Committee on Immunization Practices). Since 2020, Dr. Beysolow has served as an educator and Chair of the EPIC Immunization Advisory Committee for the Georgia Chapter of the American Academy of Pediatrics, educating health care providers across the state of Georgia on immunizations and also serves as the Georgia Chapter’s Immunization Representative to the National AAP.
Laurence S. Sperling, MD, FACC, FAHA, FACP, FASPC, Executive Director, Million Hearts Initiative, Division of Heart Disease and Stroke Prevention Centers for Disease Control and Prevention and the Center for Medicare and Medicaid Services
Dr. Laurence S. Sperling is the Executive Director of the Million Hearts Initiative for the Division of Heart Disease and Stroke Prevention at the Centers for Disease Control and Prevention and the Center for Medicare and Medicaid Services. He is the Founder and was the Director of The Heart Disease Prevention Center at Emory Healthcare. Dr. Sperling is currently the Katz Professor in Preventive Cardiology at the Emory University School of Medicine, and Professor of Global Health in the Rollins School of Public Health. He served as the President of the American Society for Preventive Cardiology from 2014-2016, served on the writing committee of 2018 the ACC/ AHA Guideline on the Management on Blood Cholesterol, and served as Chair of the World Heart Federation writing group on the Roadmap for Cardiovascular Disease Prevention among People Living with Diabetes. Dr. Sperling was the recipient of the 2017 Award of Honor from the Alumni Association of Emory University School of Medicine. He has received awards for excellence in teaching (including 4 Golden Apple Awards and The Dean’s Teaching Award), mentorship (Emory SOM 2018 Mentorship Award), and the R. Wayne Alexander Research mentor award. He has authored over 350 manuscripts/ abstracts/ books, and has been an invited speaker on every continent except Antarctica.
Moderator:
Kristen Hobbs, MPH, CPH, Director, Quality Improvement & Equity, Center for Sustainable Health Care Quality and Equity, National Minority Quality Forum
Kristen Hobbs is responsible for the oversight of quality improvement and education projects for a variety of therapeutic areas. A senior-level public health professional with experience in epidemiology, public health program evaluation, public health program development and implementation, and partnership development, Kristen is proud to champion the advancement of health equity and believes in the value of implementing epidemiologic principles for the design, implementation, and management of evidence-based public health interventions. Before joining NMQF/SHC, Kristen worked at Susan G. Komen Headquarters as Senior Manager of the African American Health Equity Initiative. She served at Komen for five years and held varying roles as an evaluator and subject matter expert in the development and implementation of the initiative. Prior to Komen, Kristen worked with the Institutional Review Board and Institutional Animal Care and Use Committee of Saint Louis University on accreditation efforts, survey development, research, and analysis. She also worked for the Saint Louis County Department of Public Health’s Communicable Disease Control Services Division to evaluate and monitor the department’s perinatal hepatitis B program, conduct epidemiologic surveillance of infectious diseases, and refine behavioral health marketing messages for STD prevention and awareness in north St. Louis, Missouri. Kristen earned her Bachelor of Science in Biology and Chemistry from Texas Woman’s University and her Master of Public Health in Epidemiology from Saint Louis University.
Sources
- Aggarwal, R., Chiu, N., Wadhera, R. K., Moran, A. E., Raber, I., Shen, C., Yeh, R. W., & Kazi, D. S. (2021). Racial/ethnic disparities in hypertension prevalence, awareness, treatment, and control in the United States, 2013 to 2018. Hypertension, 78(6), 1719–1726. https://doi.org/10.1161/hypertensionaha.121.17570
- American Heart Association News. (2021, February 23). Cold and flu medications can increase blood pressure. www.heart.org. Retrieved July 14, 2022, from https://www.heart.org/en/news/2018/05/01/cold-and-flu-medications-can-increase-blood-pressure#:~:text=The%20flu%20can%20have%20serious,to%20the%20American%20Heart%20Association.
- American Heart Association. (2021, September 17). What is high blood pressure? www.heart.org. Retrieved July 14, 2022, from https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/what-is-high-blood-pressure
- American Heart Association. (2022, June 2). Understanding blood pressure readings. www.heart.org. Retrieved July 14, 2022, from https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings
- American Heart Association. (n.d.). National Hypertension Control Initiative: Printable Resources. Downloads | NHCI English. Retrieved July 18, 2022, from https://nhci.heart.org/downloads/
- Bress, A. P., Cohen, J. B., Anstey, D. E., Conroy, M. B., Ferdinand, K. C., Fontil, V., Margolis, K. L., Muntner, P., Millar, M. M., Okuyemi, K. S., Rakotz, M. K., Reynolds, K., Safford, M. M., Shimbo, D., Stuligross, J., Green, B. B., & Mohanty, A. F. (2021). Inequities in hypertension control in the United States exposed and exacerbated by Covid‐19 and the role of home blood pressure and virtual health care during and after the Covid‐19 pandemic. Journal of the American Heart Association, 10(11). https://doi.org/10.1161/jaha.121.020997
- Cdc. (2022, May 18). “live to the beat” campaign partner toolkit: Million hearts®. Million Hearts. Retrieved July 21, 2022, from https://millionhearts.hhs.gov/partners-progress/partners/live-beat-campaign-toolkit.html
- Centers for Disease Control and Prevention. (2022, February 17). Vaccines indicated for adults based on medical indications. Centers for Disease Control and Prevention. Retrieved July 14, 2022, from https://www.cdc.gov/vaccines/schedules/hcp/imz/adult-conditions-shell.html
- Ferdinand, K. C., & Brown, A. L. (2021). Will the 2021 USPSTF hypertension screening recommendation decrease or worsen racial/ethnic disparities in blood pressure control? JAMA Network Open, 4(4). https://doi.org/10.1001/jamanetworkopen.2021.3718
- Ferdinand, K., Batieste, T., & Fleurestil, M. (2020). Contemporary and future concepts on hypertension in African Americans: Covid-19 and beyond. Journal of the National Medical Association, 112(3), 315–323. https://doi.org/10.1016/j.jnma.2020.05.018
- Mayo Foundation for Medical Education and Research. (2021, July 1). High blood pressure (hypertension). Mayo Clinic. Retrieved July 14, 2022, from https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/syc-20373410
- Mueller, M., Purnell, T. S., Mensah, G. A., & Cooper, L. A. (2014). Reducing racial and ethnic disparities in hypertension prevention and control: What will it take to translate research into practice and policy? American Journal of Hypertension, 28(6), 699–716. https://doi.org/10.1093/ajh/hpu233
- Patient-Centered Outcomes Research Institute. (2022, April 25). Minority health month: Spotlight on hypertension. PCORI. Retrieved July 18, 2022, from https://www.pcori.org/blog/minority-health-month-spotlight-hypertension
- Patient-Centered Outcomes Research Institute. (2022, April 25). Minority health month: Spotlight on hypertension. PCORI. Retrieved July 18, 2022, from https://www.pcori.org/blog/minority-health-month-spotlight-hypertension
- Peng, M., He, J., Xue, Y., Yang, X., Liu, S., & Gong, Z. (2021). Role of hypertension on the severity of COVID-19: A Review. Journal of Cardiovascular Pharmacology, 78(5). https://doi.org/10.1097/fjc.0000000000001116
- Swamy, S., Koch, C. A., Hannah-Shmouni, F., Schiffrin, E. L., Klubo-Gwiezdzinska, J., & Gubbi, S. (2022). Hypertension and COVID-19: Updates from the era of vaccines and variants. Journal of Clinical & Translational Endocrinology, 27, 100285. https://doi.org/10.1016/j.jcte.2021.100285

