Defining Cancer
- The National Cancer Institute (NCI) defines cancer as “a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body. [It] may start almost anywhere in the human body, which is made up of trillions of cells”
- Usually, when cells are abnormal or old, they die. Cancer begins when something goes wrong in this process and cells keep making new cells and the old or abnormal cells don’t die
- Causes of cancer developing may include genetics, lifestyle habits, and exposure to cancer-causing agents around you. Often, there is no clear and obvious reason.
More About Cancer
- Blood Cancers
- Cancers of the blood cells
- Solid Tumor Cancers
- Cancers of any other body organs or tissues
- Tumor
- A lump or growth
- Some are cancerous (malignant)
- Some are not cancerous (benign)
- Cancer Staging
- Important for choosing the right treatment options for each patient
- Understands size and location(s) of cancer
- Lower stages (stages 1 and 2)
- Higher stages (stages 3 and 4)
- Stage 4 is the highest and means that the cancer has metastasized/spread
Cancer Metastasis/Spread
- Metastasis happens when cancer spreads from its original location (primary site)
- If cancer cells break away from the original tumor, they may use the bloodstream or lymph system to travel to other places in the body
- Most of these cells die before they get to a new location
- However, some may begin growing in another location
- This is metastasis
Resources About Cancer
Vaccine-Preventable Cancers
- Some cancers are preventable through vaccinations
- The U.S. Food and Drug Administration (FDA) has approved two types of routine childhood vaccines for the prevention of cancer
- The HPV (human papillomavirus) Vaccine prevents cancers cervical, vaginal, vulvar, and anal cancers, and genital warts
- HPV may also cause oral cancers, for which there is no vaccine
- The Hepatitis B Vaccine protects against the hepatitis B virus that can cause liver cancer
Human Papillomavirus Vaccine (HPV)
- Human Papillomavirus (HPV) causes more than 13 million new infections each year that can lead to six different types of cancer (cervical, vaginal, vulvar, penile, anal, and oropharyngeal)
- HPV is spread through intimate skin-to-skin contact with an infected individual
- HPV vaccine was first recommended for administration to adolescent females in 2006. The recommendation was expanded in 2011 to vaccinate all males and females at ages 11-12, but can be administered as early as age 9
- Since the first recommendation in 2006, infections with HPV have decreased 88% among teen girls and 81% among young women
- The vaccine is among the most effective ever developed. Clinical trials found the vaccine to be nearly 100% effective in preventing cervical, vulvar, and vaginal infections and precancers caused by all seven cancer-causing HPV types
- Younger people develop a greater immune response to the vaccine, which prompted a reduction in the number of doses needed. Adolescents who initiate the series before the 15th birthday need 2 doses; those who begin after the 15th birthday need 3 doses. Studies have shown no reduction in protection over time.

Hepatitis B Vaccine (HepB Vaccine)
- Hepatitis B Virus causes liver disease that can be mild, but can become chronic and result in liver damage (cirrhosis), liver cancer, and death
- HepB vaccine is spread through contact with infected body fluids or transmitted from mother to fetus. It is primarily spread through injected drug use and sexual contact.
- HepB vaccine was first recommended for administration to all newborns in 1991 in an effort to eliminate hepatitis B infections. The vaccine, along with hepatitis B immune globulin (HBIG), is also given to newborns of hepatitis B+ mothers to prevent infection.
- Hepatitis B cases declined 88.5% since recommendations for HepB vaccination were first issued. 95% of newly reported chronic infections in the U.S. are now from foreign-born persons
- 80-90% of persons infected during infancy will develop chronic infection. Approximately 25% of them will die prematurely from cirrhosis or liver cancer
- The 3-dose HepB vaccine series protects approximately 95% of healthy infants and >90% of health adults aged <40 years.
Cancer and Vaccine Resources
Inequities in Cancer Outcomes
Disparities & Inequities
- Disparities are differences/gaps in cancer incidence and outcomes based on factors such as race, ethnicity, age, income, sexual orientation, gender identity, and where one might live
- According to the American Public Health Association (APHA), “inequities are created when barriers prevent individuals and communities from accessing [high quality healthcare] and reaching their full potential. Inequities differ from health disparities, which are differences in health status between people related to social or demographic factors such as race, gender, income or geographic region. Health disparities are one way we can measure our progress toward achieving health equity”
Cancer Measures Affected by Disparities

- Incidence (new cases)
- Prevalence (all existing cases)
- Mortality (deaths)
- Survival (how long people survive after diagnosis)
- Morbidity (cancer-related health complications)
- Survivorship (including quality of life after cancer treatment)
- Financial burden of cancer or related health conditions
- Screening rates
- Stage at diagnosis
- Cancer disparities can also be seen when outcomes are improving overall but the improvements are not seen in some groups relative to other groups.
Disparities Along the Cancer Continuum
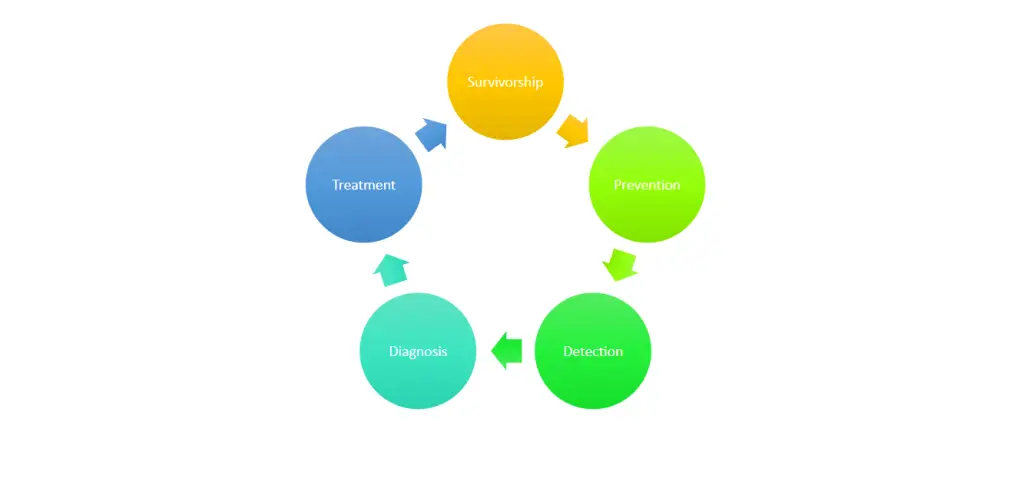
Disparities may occur across the cancer continuum of care.
Racial & Ethnic Inequities
- Black men have the highest overall cancer mortality rate at 221 per 100,000 people
- Prostate cancer mortality in Black men is more than double that of any other racial or ethnic group
- Black women have a 41% higher breast cancer death rates than white women, even though both groups have similar incidence rates
- Disproportionate poverty due to systemic racism that reduces access to equitable care contribute to disparities in cancer survival rates

Racial & Ethnic Inequities

Black men have the highest overall cancer mortality rate at 221 per 100,000 people
Prostate cancer mortality in Black men is more than double that of any other racial or ethnic group
Black women have a 41% higher breast cancer death rates than white women, even though both groups have similar incidence rates
Disproportionate poverty due to systemic racism that reduces access to equitable care contribute to disparities in cancer survival rates
Cancer Inequities in Asian and Pacific Islander Populations
- In Asian and Pacific Islander populations, cancer is the leading cause of death in the US
- Asian and Pacific Islander populations have the double the rates of liver and stomach cancer as that in white populations
- Due to historically high smoking prevalence, Native Hawaiian populations have higher rates of lung cancer than white people
- Variations in cancer occurrence within the Asian and Pacific Islander population reflects diversity in geographic origin, language, acculturation, and SES
- Current cancer data is largely unavailable for individual Asian and Pacific Islander populations

Hispanic and Latino Populations
- Cancer is the leading cause of death among Hispanic and Latino populations
- Hispanic and Latino populations have the highest rates of cancer associated with infectious agents – cervical cancer, liver cancer, and stomach cancer
- Rates for the most common cancers – female breast, colorectum, lung, and prostate – are lower for Hispanic and Latino populations
- Cancer rates vary according to country of origin, generation, birthplace, and duration of residence in the US (acculturation)
Achieving Health Equity
- In order to achieve health equity, we must be invested in reducing patient risk and providing everyone with the optimal opportunity to be their healthiest self
- The APHA has outlined some ways for reaching this goal
- Valuing people equally
- Optimize the conditions in which people are born, grow, live, work, learn, and age
- Work with other sectors to address the factors that influence health, including employment, housing, education, health care, public safety, and food access
- Name racism as a force in determining how these social determinants are distributed
Inequities in Cancer Outcomes Resources
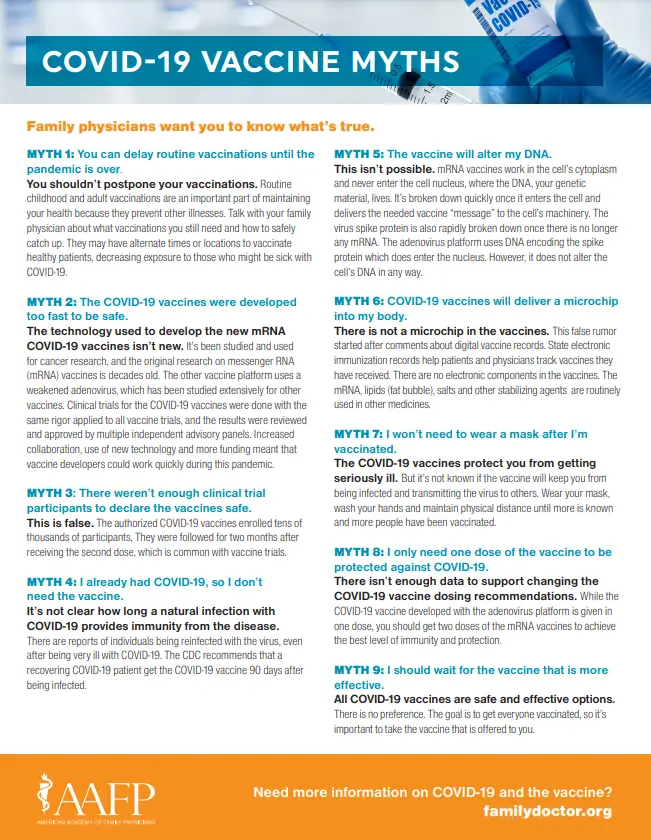
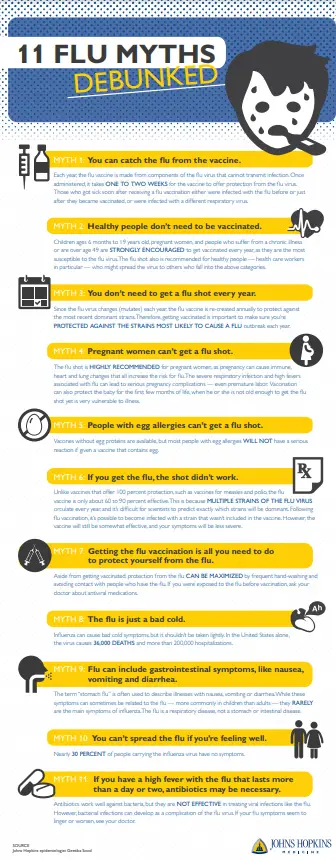
Flu & COVID-19 + Cancer
Flu Vaccination + Cancer
- The CDC recommends everyone 6 months and older get a flu shot each year
- People living with cancer should be vaccinated against the flu with the shot that has an inactive (dead) virus annually
- However, people with cancer should NOT get the nasal mist flu vaccine, as it contains a weakened version of the live virus
- People who live with (including children) or are caregivers of a person with cancer and is at high risk for flu-related complications should get vaccinated against the flu
- Consult with your clinical team if you have more questions

COVID-19 Vaccination + Cancer

- The National Comprehensive Cancer Network (NCCN) recommends that all patients living with cancer and cancer survivors be vaccinated against COVID-19 as soon as they can, plus additional booster doses
- Some cancer treatments that affect the immune system might make the vaccine less effective
- People with certain types of cancers (ex. leukemias or lymphomas) can also have weakened immune systems, which may make the vaccine less effective
- People with certain types of cancers (ex. leukemias or lymphomas) can also have weakened immune systems, which may make the vaccine less effective
- Given this, the NCCN and the CDC recommend that people with cancer who have a weakened immune system should get 3 doses of one of the mRNA COVID-19 vaccines as the primary series, plus an additional 2 booster doses (for a total of 5 shots)

- For people with cancer who do not have a weakened immune system, the NCCN and the CDC recommend 2 doses of an mRNA COVID-19 vaccine or one dose of the Janssen vaccine, plus an additional booster dose
- Always talk to your doctor if you have cancer, to help you determine your immune status.
Vaccine Recommendations for Cancer Survivors
- It’s generally recommended that vaccines not be given during chemo or radiation treatments – the only exception to this is the flu shot. This is mainly because vaccines need an immune system response to work, and you may not get an adequate response during cancer treatment.
- People with cancer who have a weakened immune system should get 3 doses of one of the mRNA COVID-19 vaccines as the primary series, plus an additional 2 booster doses (for a total of 5 shots)
- For people with cancer who do not have a weakened immune system, the NCCN and the CDC recommend 2 doses of an mRNA COVID-19 vaccine or one dose of the Janssen vaccine, plus an additional booster dose
- People living with cancer should be vaccinated against the flu with the shot that has an inactive (dead) virus annually
- People who have weak immune systems should not get the measles-mumps-rubella (MMR) vaccine because it contains live virus. But it’s safe for other household members to get it. If needed, your doctor may consider giving you the vaccine before cancer treatment starts

- The pneumococcus vaccine can help people with weak immune systems fight off certain lung, blood, or brain infections caused by certain bacteria. Ask your doctor if you need to receive the pneumococcal vaccine and when you need to get it
- The meningocoocal vaccines (MenACWY and MenB) help prevent meningococcal disease, which can cause meningitis or other infections. This vaccine should not be given during cancer treatment. It may be offered before treatment, or after the patient’s immune system has recovered. In cases where a patient is having the spleen removed, this vaccine may be given before surgery. Talk to your doctor to see if and when you may need to receive the meningococcal vaccines
- The polio vaccine is used to prevent polio, a viral infection linked to severe illness and physical disability. Since the vaccine came out in 1955, polio has been eradicated from much of the world and there has not been a reported case in the U.S. since 1979*
- Children who have weak immune systems, as well as their siblings and others who live with them, only should get inactivated polio virus vaccines. Most doctors in the United States use only the inactivated polio vaccine, but you should ask to be sure in case the child received vaccinations outside of the US


- The varicella vaccine is intended to prevent chickenpox in people who have never had it. This is a live virus vaccine. It should not be given to people with weak immune systems, or to people with leukemia, lymphoma, or any cancer of the bone marrow or lymphatic system unless it’s treated and under control. It’s OK for household members of the person with weak immunity to get the varicella vaccine. If a vaccinated person develops a rash, it is recommended that close contact with persons who do not have evidence of varicella immunity and who are at high risk of complications of varicella, such as immunocompromised persons, be avoided until the rash has resolved. Talk to your doctor for more information or if you have questions
- The shingles vaccine is given to adults age 50 and older who have had chickenpox or shingles in the past to help prevent shingles or make symptoms of shingles less severe. If you have a weak immune system from cancer or cancer treatment, talk to your doctor about chicken pox and shingles vaccine options and whether one of these vaccines might be right for you
Cancer + Vaccine Resouces
Vaccine Myths/Misconceptions
See pdfs for flu and COVID-19 to upload.
Watch Now: Cancer + Vaccines
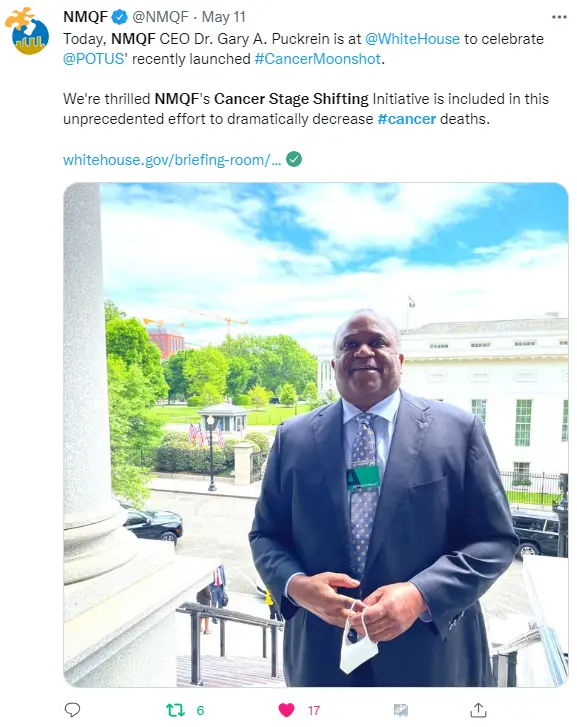
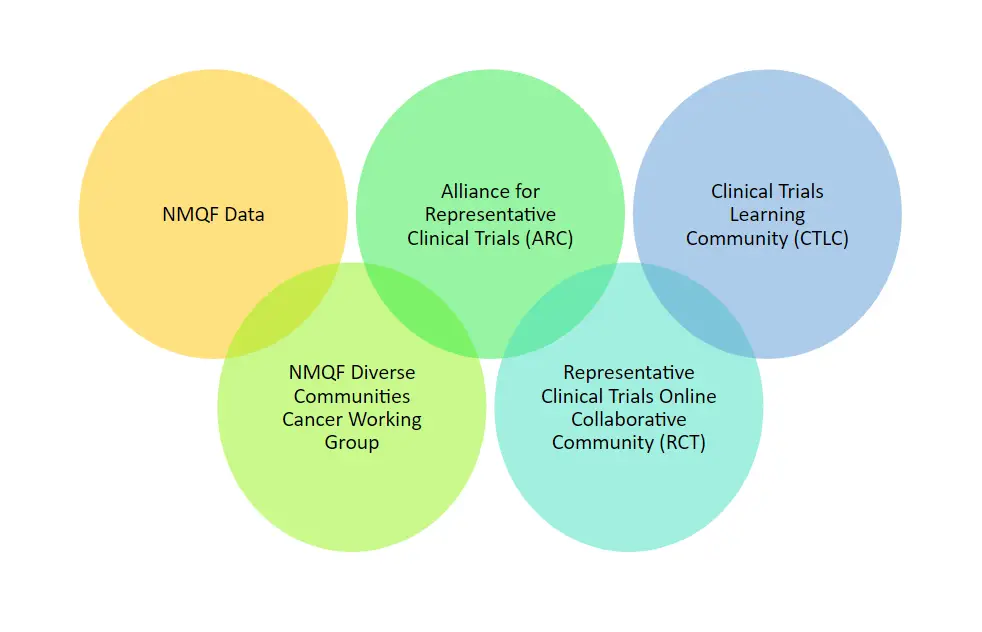
NMQF Cancer Work
- Promote adoption of actionable CWG Cancer Indices
- Address cancer health equity in high-risk communities
- Increase Diversity in Cancer Research
- Drive Community and Patient Engagement
- Special Focus for 2022: Engaging the Medicaid population and new Cancer Moonshot Initiative
- Involvement in the Cancer Moonshot

Cancer Index
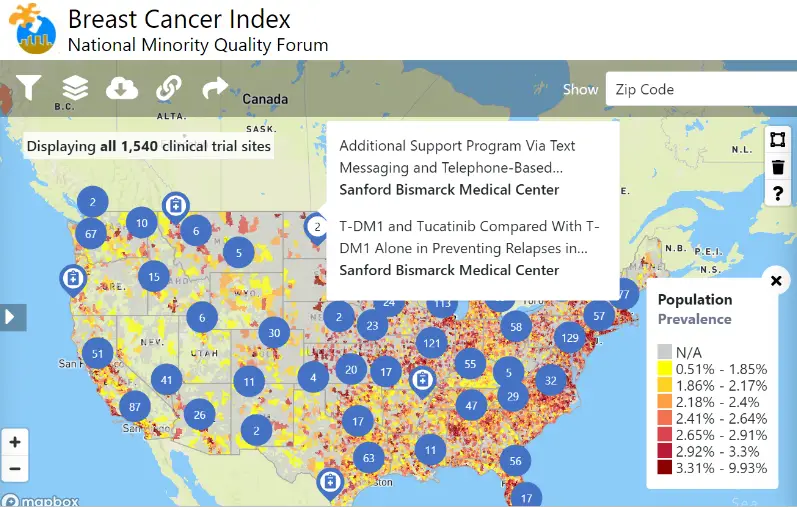
- Over 5 billion CMS patient records to define disease prevalence, costs and outcomes for demographic subpopulations by geography (zip code, state, country, congressional and state legislative districts
- Continuous integration of additional data and overlays
- Medicaid, 2015-2018
- Medicare FFS, 2015-2019
- Clinical Trial site overlay (via clinicaltrials.gov)
- Quest Diagnostics site overlay (in production, April 2022)
- Cancer
- Breast Cancer
- Colorectal Cancer
- Endometrial Cancer
- Lung Cancer
- Prostate Cancer
- Skin Cancer
Cancer Stage Shifting Initiative
Mission: Move from late stage to early-stage diagnosis and treatment of cancer, improving cancer care and reducing the incidence of cancer deaths for all, with a particular focus on equity and underrepresented populations
Involve all sectors at NMQF
Partner with industry leaders to bring to fruition
Build on the notion of collective action networks
Representative Clinical Trials
A peer-to-peer online, collaborative community for clinical development professionals and advocates to build capabilities to create and perform best practices, strategies and interventions that deliver representation in clinical research. Focus on curating the best tools, toolkits, and research to facilitate peer support and expert guidance to help individuals and organizations adapt to the needs of diverse populations when designing and conducting clinical research
More Resouces
Risk Mitigation Strategies
- Continue wearing a mask indoors and in large outdoor gatherings
- Engage in good hand washing and hand hygiene
- Remain physically distant when around people who do not live with you
- Engage in stress management tactics, including self-care, meditation, and therapy
- Engage in eating nutrient-dense foods and regular exercise
- Get regular fresh air

Sources
- American Cancer Society. Cancer Facts & Figures 2022. Atlanta: American Cancer Society; 2022
- Cancer care continuum. Public Health Sciences Division. (2021, February 24). Retrieved June 21, 2022, from https://publichealthsciences.wustl.edu/research/faculty-projects-2/cancer-care-continuum/
- Cancer disparities. National Cancer Institute. (n.d.). Retrieved June 21, 2022, from https://www.cancer.gov/about-cancer/understanding/disparities
- Covid-19 vaccines in people with cancer. American Cancer Society. (n.d.). Retrieved June 20, 2022, from https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/low-blood-counts/infections/covid-19-vaccines-in-people-with-cancer.html
- Health Equity. American Public Health Association (APHA), Health equity. (n.d.). Retrieved June 17, 2022, from https://www.apha.org/topics-and-issues/health-equity
- Vaccinations and flu shots: Vaccinations during cancer treatment. American Cancer Society. (n.d.). Retrieved June 20, 2022, from https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/low-blood-counts/infections/vaccination-during-cancer-treatment.html
- What are cancer vaccines? Cancer.Net. (2021, December 23). Retrieved June 16, 2022, from https://www.cancer.net/navigating-cancer-care/how-cancer-treated/immunotherapy-and-vaccines/what-are-cancer-vaccines#:~:text=The%20FDA%20has%20approved%20HPV,Anal%20cancer
- What is cancer? National Cancer Institute. (2021, May 5). Retrieved June 14, 2022, from https://www.cancer.gov/about-cancer/understanding/what-is-cancer#:~:text=Pittsburgh%20Cancer%20Institute-,The%20Definition%20of%20Cancer,up
%20of%20trillions%20of%20cells. - What is cancer?: Cancer basics. American Cancer Society. (2022, February 14). Retrieved June 16, 2022, from https://www.cancer.org/treatment/understanding-your-diagnosis/what-is-cancer.html