
No person living with cancer should be at a higher risk for complications, disabilities and death because of who they are or the conditions in the places where they live, learn, work, and play – also known as social determinants of health – do affect health and access to health care. Other structural and social factors include financial security, education, access to food, social support, and discrimination.
People of color face disproportionate barriers in oncology, which is why Lilly and the National Minority Quality Forum (NMQF), a research and educational organization dedicated to ensuring high-risk populations receive optimal health care, are working together to reimagine cancer care.
Together, we’ve developed Opportunities to Improve Quality & Advance Equity Along the Cancer Care Continuum, a detailed paper that outlines existing health disparities and provides guidance and recommendations for improving care among all those impacted by this complex disease.
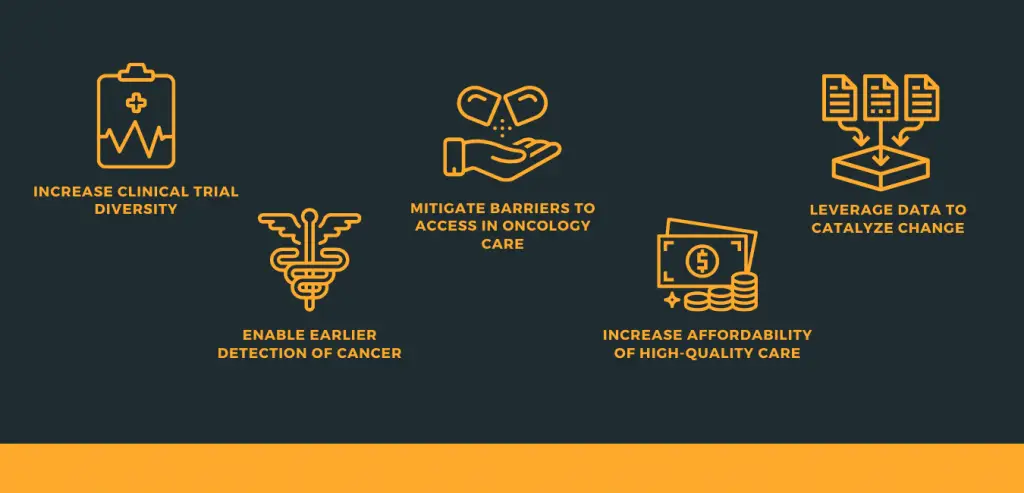
Increase Clinical Trial Diversity
Clinical trials in oncology are crucial for developing new treatments and give cancer patients the opportunity for early access to lifesaving therapies. However, nearly 75 percent of cancer patients will not have the option to enroll in a local clinical trial due to socioeconomic status. For widespread change in this area, researchers need to modify study criteria.
Enable Earlier Detection of Cancer
Ethnic and racial minorities are more likely to be diagnosed with cancer at a later stage, resulting in higher death rates. Increasing access to these populations through public and private insurance – as well as opportunities for early detection of the disease – are imperative.
Mitigate Barriers to Access in Oncology Care
Americans living in rural and/or low-income areas are more likely to die from cancer than those living in urban areas. Long travel distances to medical facilities for screenings and treatment and a lack of health insurance are examples of obstacles these people can face. We need to ensure those living with cancer have access to additional services such as transportation and care coordination assistance.
Increase Affordability of High-Quality Care
Even for those with insurance, medical and non-medical costs for cancer patients are a significant burden. Policy reforms are required for better insurance design options that improve access to healthcare with lower deductibles and patient out-of-pocket costs.
Step therapy, also known as “fail first” policies, used by health plans could limit access to prescribed treatments. Promoting standards of care and clinical guidelines along with adherence programs that connect patients to resources and support could help lower costs.
Leverage Data to Catalyze Change
Despite tremendous advances in health record collection and analysis of race, income, and other data about cancer prevalence and care utilization, providers often lack knowledge of their patients’ non-clinical needs.
Making this data available to identify needs and barriers to care is the first step. Using that data to drive decision-making for patient care is next.
Exploring and monitoring data is also important in the work to expand digital and telehealth treatments for chronic conditions – with appropriate reimbursement from insurance, this is a growing option for care.
Working alongside partners, like Lilly, we are committed to collaborating across the healthcare and cancer communities to discuss, advocate, and build solutions to affordability, access, and wide-ranging health disparities, so our oncology advancements have meaning for all people living with cancer.
We support reforms that improve care to the underserved through enhanced language access services, train providers on cultural competency, and increase investments in diversifying the workforce, among many other changes.
We believe reimagining equitable high-quality cancer care is achievable.